Can e-Health Scale in Africa?
~9 min read

Two years after the start of the pandemic, a groundswell of healthcare electrification and digitization investments is preparing to crest. This is certainly not the first time that the global community of technologists, financiers, and governments rally behind the modernization of health systems at all levels. What may be different from previous responses to health catastrophes, however, is the more central role that digital connectivity, mobile money and fintech is to play not only in ensuring the basics of health facilities — like lights for night-time operations — but also in converting the flow of electrons through facilities’ outlets into more efficient systems, processes, and outcomes. Yet despite universal acknowledgment of the importance of digitizing health, there remains significant research gaps in terms of what works and what doesn’t as far as implementation and scale is concerned. What has become clear is that single issue-focused solutions – like addressing Ebola, COVID-19 or just electrification – are not only difficult to scale but may also contribute to increasingly fragmented systems that don’t “talk” to one another, adding confusion to an already under-resourced sector.
Glimpse From Central Africa
At a hospital on the outskirts of Goma, the provincial capital of the infrastructurally-challenged eastern Democratic Republic of the Congo, a technician explains the challenges he faces in keeping the lights on at the hospital from his office, a repurposed shipping container packed with broken oxygen tanks, fans, sterilizers and other half-stripped equipment. “Normally, our job as technicians should be to just show up to the hospital and make sure everything is working,” he says. “But because of the situation, we must be here every day, all the time. If the power is cut and they are in town, it can take 30 minutes to an hour for the technician to come and get the power working again.
A nurse shows up to his office and requests some AAA batteries for an oximeter. The technician pulls a pack out of his desk. Batteries bought at local markets can be such poor quality that they ruin the device, he remarked. With replacements taking months to come, they try to reuse parts whenever possible.
The grid cuts unexpectedly, and as the technician makes his way to the control room, he makes a mental decision about which hospital units will use how much electricity for this time of the day. At the control room, he pulls the levers and flips the switches that reroute power intake from the onsite generator to the prioritized hospital units. “The laboratory will complain,” he says, but he knows it is a particularly busy time in intensive care.
While years of experience have made this technician an expert in such a weighty calculus, it remains a dangerously heuristic process. Indeed, as Damilola Ogunbiyi, CEO and Special Representative of the UN Secretary-General for Sustainable Energy for All and Co-Chair of UN-Energy, recently noted in a conference on healthcare electrification and telecommunication, when it comes to power in health facilities, “seven seconds is the difference between life or death, particularly for infants and mothers.”
Behind these visceral gaps lies the more humdrum aspects of healthcare services where digitization manifests: having a digital database where patient records can be kept and updated, insurance forms for tracking payments, or automatic bill-pay for recurring hospital bills for things like electricity, water, and sanitation. SillonDMS is a young startup also based in Goma that offers such digitization of records through a 100-page-per-minute scanner and an integrated cloud functionality for archive organization. A local hospital is among the clientele for this service that promises to digitize years and years’ worth of notebooks collecting dust — it will take some time, effort, and money. But management clearly sees a return on investment in terms of the efficiency of operations.
Powering Digital Health
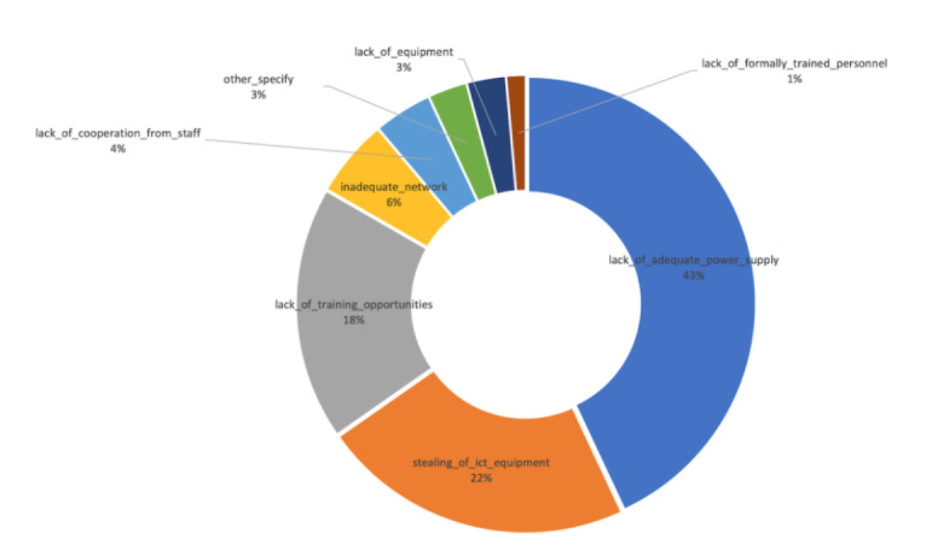
Digital connectivity in hospitals like these, where power outages from the national grids are common, is several degrees removed from the daily reality of simply keeping the power flowing long enough to patch up patients’ injuries, deliver babies and perform surgery. The situation is far from uncommon; a recent study of 72 health facilities in Sierra Leone investigating the role of tablets and computers, electricity and Internet in digitizing health operations, found that inadequate electricity is by far the biggest threat to digitization.
Gaining access to electricity represents only the first step in the digitization process, for healthcare facilities as well as households and businesses. Yet basic information about the state of electrification in such critical facilities in emerging markets remains relatively sparse; the most widely cited study on the intersection of power and health in Africa, for example, dates back to a 2013 literature review synthesizing 13 health facility surveys from 11 countries on the continent. The results, widely cited to this day, paint a grim picture: less than a third of health facilities on the continent were estimated to experience reliable electricity, while just over a quarter were characterized as having no electricity supply at all.
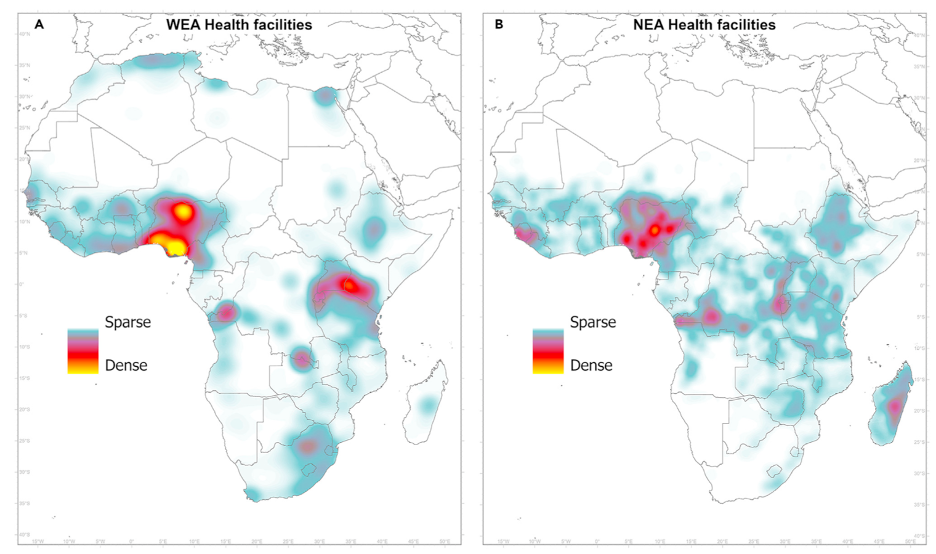
Source: Moner-Girona et al. (2021) Achieving universal electrification of rural healthcare facilities in sub-Saharan Africa with decentralized renewable energy technologies; (A) facilities with detected electricity access (WEA) and, (B) facilities with no detected access to electricity (NEA).
eHealth or eHype?
This reality contrasts starkly with the growing momentum around digital health initiatives, which was explicitly adopted as a resolution by the World Health Organization’s Africa Region in 2013. Fast forward to late 2020, with the world well into the worst pandemic in a century, and almost all African countries had formally launched some kind of national digital health strategies and architectures. Only 12 countries, had demonstrated any kind of implementation for these strategies, however.
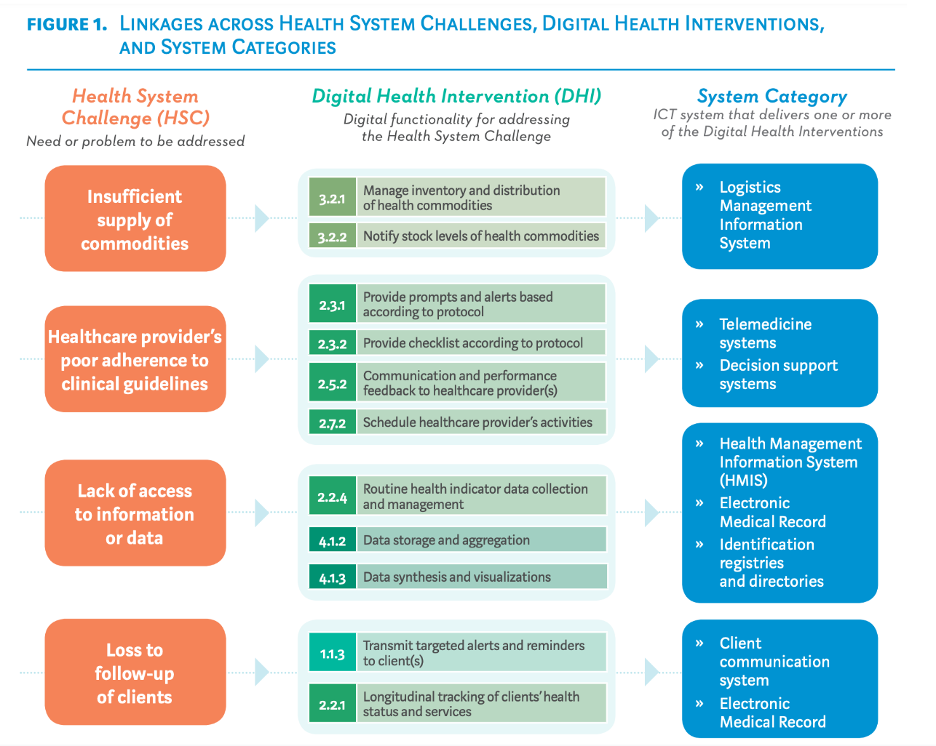
Source: WHO (2018) Classification of Digital Health Interventions v 1.0
Indeed, digital health initiatives, despite their universally acknowledged importance to social and economic development in the region with many of the world’s worst healthcare outcomes, have struggled to scale in any kind of systematic fashion. Despite record-topping investments in African health startups and biotech startups — nearly $400 million in funding in 2021, an 81% increase from 2020, according to Briter Bridges — this represents a paltry 8% of total funding in the technology sector in Africa, compared to a whopping 62% for fintech.
This is not to dismiss the innovations in health technology that have made headway before and through the pandemic. The Brookings Institute catalogs a number of success stories that span the spectrum of Fourth Industrial Revolution technologies: Uganda’s public-private mTrac partnership for digitizing health data reporting, verification, and analysis, leveraging SMS-based reporting systems, includes more than 60,000 healthcare workers in its database and aims to scale to 300,000. 3D printing companies in Kenya stepped up to fill the personal protective equipment shortage. Zipline drones in Rwanda, Ghana and Nigeria continue to innovate in aerial deliveries of medical supplies like vaccines and blood to remote regions.
Fintech, mobile money and other telecom-dependent players have proven critical to the success of many such eHealth innovations, and it is clear that both feature phones and smartphones will continue to form the material base of the networks connecting patients to increasingly digitized healthcare systems. Call record data, the continued proliferation of mobile wallets and smartphones among younger populations will inevitably continue to mainstream digital health solutions into more patients’ pockets.
See, for example, the success of M-Tiba, a self-described “health financing technology platform” out of Kenya that offers healthcare providers a system of combining digital payments with ‘real time’ medical and financial data. Claiming almost 5 million users across Africa, the platform offers users the ability to save any amount of funds in their mobile account, pay, and get treated by healthcare providers contracted directly through the company. Streamlining the payment and processing systems of notoriously bureaucratic insurance systems has proven a real market need, and partnerships with both governments and private insurers has created entry points for the various actors involved in a health system to move from pen-and-paper processes to a more efficient, digitized one.
Such confidence-inspiring trends prompted The Lancet, one of the world’s preeminent academic journals in the health space, to declare in a 2020 article that with the “increased use of digital health solutions and interventions for clients, health-care providers, health-system managers, and data services…sub-Saharan Africa is booming with digital health.”
Yet when it comes to structurally addressing vulnerable health systems, individual success stories are not enough. Recent research on digital health in East Africa puts it bluntly: “despite the optimism for digital technologies for health and healthcare, there is not yet evidence that they are helping to produce stronger or more affordable national healthcare systems.” A 2020 Nature Digital Medicine article reviewing the impact evidence for the WHO’s “first-ever evidence-based guidelines for digital health” is similarly concerning: on the WHO’s nine recommendations on selecting digital health interventions that involve the use of a mobile phone or device, the research starkly highlights for each “a continued dearth of robust evidence” for benefits wrought.
Data To Deliver
With COVID-cases resurging in many parts of the world, significant supply chain challenges in getting temperature-sensitive vaccines to power-constrained health facilities and just 7.5% of Africa’s population fully vaccinated, the ‘boost’ the pandemic provided to different aspects of healthcare digitization, particularly around telemedicine and mobile data for COVID-tracking, is yet to deliver satisfactory results in terms of truly catalyzing more modern health systems. A new initiative, called the Healthcare Electrification and Telecommunication Alliance (HETA), aims to tackle these scale challenges by focusing on the “base” infrastructure for digital health: stable power and Internet connectivity.
Such a two-pronged approach should provide additional fuel for the acceleration of mobile money, which remains relatively limited in places like the eastern Congo, despite the ubiquity of airtime vendors under parasols along busy roundabouts in provincial capitals and secondary cities. Research utilizing phone record data from Orange in Senegal found that access to mobile connectivity for rural users, measured by mobile telephony subscriptions or smartphone ownership, increases with access to electricity, with a stronger impact for women. Extending this inclusion logic to focus on health facilities, then, should represent a significant opportunity to provide evidence for strong social impacts as a result of digital inclusion.
The alliance, composed of over 30 partners including GAVI, UNICEF, Bechtel, and Orange, will aim to reach the estimated 100,000 public health facilities in sub-Saharan Africa that lack access to reliable power and internet connectivity, starting with 10,000 in the short- to medium-term.
Dr. Daniel Kammen is a professor of Energy and Resources at the University of California Berkeley, as well as Senior Advisor for Energy Innovation to USAID, a key convener of the alliance. He reflects on what kind of approach can ensure such a massive push will result in the kinds of big, structural change that proponents of digitizing health systems envision — in particular, the kinds of data-driven decision-making that separates today’s era of real-time connectivity from previous waves of health modernization pushes:
“There is increasing recognition that what we’ve traditionally called ‘development’ can be done more effectively by leaning on new forms of data enabled by information & communications systems, and not just the “base layer” of telecoms infrastructure but all the insights and platforms that get built on top of that.”
Dr. Daniel Kammen, Professor of Energy and Resources at the University of California Berkeley, Senior Advisor for Energy Innovation to USAID
One thing that is clear from previous such efforts, however, is that in order to move from hype stories to modern health systems, there is a need for further convergence and coordination — and critically, data — across at least three distinct and technically challenging fields of expertise: power systems for reliable and quality electricity supply; digital connectivity infrastructure comprised of both traditional and next-generation mobile connectivity infrastructure for remote environments; and health sector expertise capable of identifying and implementing digitization use-cases at the facility, regional and national level.
Creating a digital paper trail from this kind of data can begin to unlock some of the integrations with digital finance services that leverage “thin-file” use-cases — for example, using mobile payment transaction data for lending, formalizing digital identities into national records, or boosting savings — all of which can contribute not just to better financial health, but physical health as well.
Yet systematic analysis of the impact evidence for the digitization of health systems indicates that treating each of these systems in siloes is doomed to result in a fragmented digital health landscape. The big challenge for a post-pandemic recovery to a more modern and just way of delivering healthcare services, then, must be interdisciplinary and holistic: much like the treatment of patients, treating individual symptoms must not obviate the need for addressing underlying conditions.
Image courtesy of National Cancer Institute
Click here to subscribe and receive a weekly Mondato Insight directly to your inbox.

Not All Fintechs Will Weather The Current Shock — And That’s A Good Thing
Mondato Summit Africa 2022: Key Themes and Takeaways